The results of a large treatment trial for hospitalised covid-19 patients funded by the World Health Organisation offer little good news. The international research found no evidence that several treatments, including the promising antiviral drug remdesivir, had any real effect on patients’ odds of survival or other outcomes.
The SOLIDARITY trial is the largest randomised, controlled study of its kind. Beginning in late March, it involved over 11,000 patients in more than 400 hospitals across 30 countries. Patients were randomly selected to receive one of four drugs in addition to standard care or simply standard care. These drugs were remdesivir; hydroxychloroquine; a combination antiviral treatment already used for HIV called lopinavir-ritonavir; and interferon β1a, a drug derived from our immune cells used to treat multiple sclerosis (initially, the interferon was given in combination with lopinavir, but that stopped after early July).
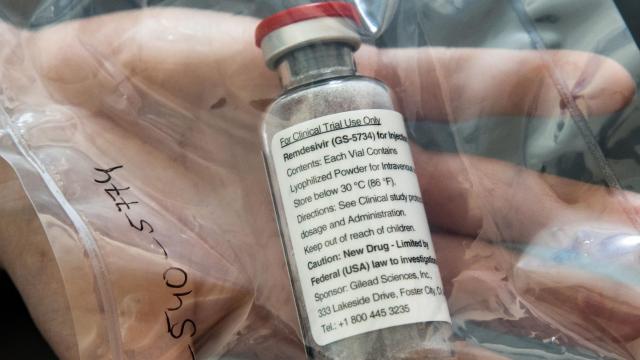
Earlier results obtained from the trial as it was ongoing had already suggested that hydroxychloroquine wasn’t effective at preventing deaths from covid-19. This eventually led to the WHO stopping that arm of the trial in June. Other studies had already suggested lopinavir-ritonavir wasn’t effective for covid-19 either, and the WHO cut short that arm of the trial in June as well. But the verdict was less certain for interferon. And in April, a relatively large trial of 1,000 patients funded by the makers of remdesivir, Gilead Sciences, seemed to provide data that remdesivir could shorten the length of symptoms from the viral illness and possibly lower mortality under certain circumstances.
However, the findings from the much larger SOLIDARITY are gloomy: None of the four drugs were associated with a significant increase in survival among patients. These drugs also didn’t seem to have any effect on reducing the need for a ventilator or in cutting short hospital stays, unlike the earlier remdesivir trial suggested.
“The main outcomes of mortality, initiation of ventilation and hospitalisation duration were not clearly reduced by any study drug,” wrote the authors of a preliminary paper on the findings, released on the preprint website medRxiv Thursday. For those who took the drugs interferon and hydroxychloroquine, there even seemed to be a small increased risk of dying, though the data isn’t certain there.
It’s worth noting that the findings still haven’t undergone a proper peer review. But outside experts have previously lauded the design of the SOLIDARITY trial, and the size of clinical trial data it’s provided is substantial. For interferon and remdesivir, the authors note, this trial accounts for more than three-quarters of all patients who have been randomised to receive them so far. In other words, though it’s possible that future trials could still find some benefit here, possibly for select groups of covid-19 patients, the big picture for any of these drugs isn’t looking great.
“For each of these 4 repurposed non-specific antivirals, several thousand patients have now been randomised in various trials,” the authors wrote. “The unpromising overall findings from the regimens tested suffice to refute early hopes, based on smaller or non-randomised studies, that any will substantially reduce inpatient mortality, initiation of ventilation or hospitalisation duration.”
As disappointing as this may be, the prospects for treating covid-19 aren’t hopeless. There have been steady improvements in the standard hospital care for covid-19 patients, as doctors have become better at knowing when patients need intensive interventions like ventilators and can more often avoid their use altogether. Other research has found a modest but meaningful life-saving effect from common steroids for severe covid-19, allowing them to be a standard treatment in those cases. And there are other experimental drugs, such as monoclonal antibodies, that have shown more promise than the drugs tested out earlier, and the WHO is now testing those as part of SOLIDARITY.
The findings do reinforce an important lesson about the pandemic, though: There’s not going to be a single miracle cure that gets us through this.