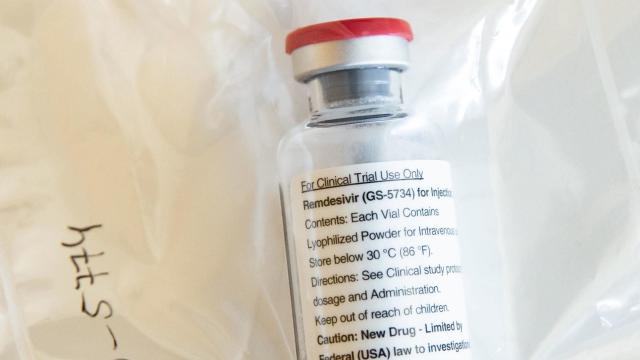
A wave of results from studies involving remdesivir, an experimental antiviral being used to treat covid-19, has arrived today. The data so far doesn’t provide a concrete answer as to how effective or life-saving the drug truly is for coronavirus patients. Nonetheless, the New York Times reports that the U.S.’s Food & Drug Administration is set to issue an emergency use authorisation for remdesivir, which would expand its availability.
This morning, the maker of remdesivir, Gilead Sciences, released a statement detailing the results of its self-funded trial of the drug. The trial involved hospitalised patients diagnosed with severe covid-19, who were separated into two groups that received either a five- or 10-day course of remdesivir. However, it did not involve a control group for comparison, something that is considered a vital aspect of high-quality drug research.
Slightly over 50 per cent of each group recovered enough to be sent home within two weeks of starting the drug, which is given through IV and is thought to work by impairing the virus’s ability to replicate. Around 8 per cent of those in the five-day treatment group died, while 11 per cent died in the 10-day group. In the 10-day group, 10 per cent of patients experienced severe enough reactions to the drug that it was discontinued.
Gilead said that these results suggest that remdesivir can be safe and possibly still effective when taken only for five days. If true, the company added, that would lengthen the available supply of the drug should it become a standard treatment for covid-19. The company also said it had received word that results from another trial of remdesivir, funded by the U.S. government’s National Institutes of Health, would be released today and that they would be positive.
Sure enough, the NIH released the basic findings from its randomised and controlled trial this afternoon. The trial, which involved over 1,000 patients with severe covid-19, found a significant improvement in the time to recovery for those taking the drug. People on remdesivir took a median length of 11 days to recover, compared to the 15 days it took for people receiving placebo.
In a press briefing today, Anthony Fauci, chief of the NIH’s National Institute of Allergic and Infectious Diseases, said that the results were “good news.” He also said that the study’s findings would be submitted to a peer-reviewed journal soon.
But the findings of the NIH trial aren’t as unequivocal as you would hope. For one, though people on remdesivir did die at a slightly lower rate than those on placebo—8 per cent compared to 11 per cent—the difference between the groups was not statistically significant.
Also today, The Lancet published data from a randomised and controlled study of remdesivir that took place in China and was accidentally released last week on the World Health Organisation’s website. The findings confirmed what was already previewed: Those on the drug did not seem to recover any quicker than those on placebo. The Lancet study also has its caveats, namely that it only enrolled 237 patients before it was ended early. Gilead has said that the trial was stopped due to a lack of eligible patients.
[referenced url=” thumb=” title=” excerpt=”]
Regardless, what we’re left with for now is a muddled picture. If the drug truly has a benefit for severe covid-19 patients, then it could be the first specific treatment for the coronavirus available. But those modest benefits may not extend to actually saving lives. It’s possible that remdesivir may be more effective when given early on in an infection rather than once a person has reached critical condition. There are other trials underway testing remdesivir on moderate covid-19 cases, so we may have insights into this soon.